
What is a provider collaborative?
NHS provider collaboratives are partnerships between two or more NHS trusts (England only). The purpose of these collaborations is for hospitals and other care services to be able to team up and use their size to better provide services or to get more value for money by buying medicines and equipment in bulk, utilising economies of scale.
The formal move from NHSE is part of a greater government and NHS push to achieve joined-up care and to have one seamless national system that has minimal wasted funding and maximum capacity for patients.
Provider collaborative governance
When provider collaborative governance was first discussed within the government’s announcement on provider collaboratives being mandated, three models were proposed as the initial default approaches to leadership and oversight – though there is flexibility to alter and adapt over time based on the needs of those collaborating.
These three models are:
- Lead Provider
- Shared Leadership
- Provider leadership board
The following graphics are sourced from the King’s Fund's own article on provider collaboratives.
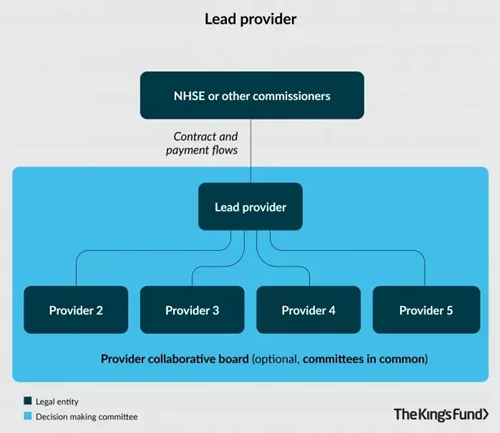
Lead Provider:
In the first example of governance, a single NHS trust handles the responsibilities of management. This ‘lead provider’ is the primary point of responsibility for contracts and the delivery of services, with the benefit being a single point of contact for NHS England or whichever body is commissioning.
The partner providers reporting to this trust all partake in a partnership agreement and typically in some form of committee or collaborative board to discuss strategy and progress.
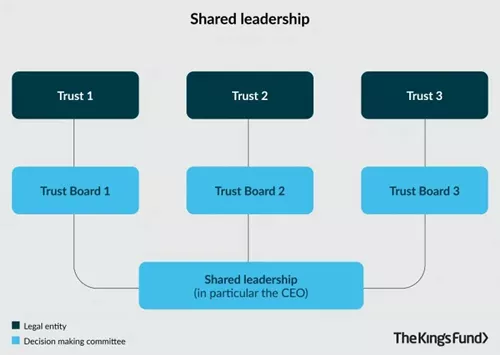
Shared Leadership:
The shared leadership approach sees all collaborating trusts report to a trust board, and then members of these trust boards report to a decision-making committee comprised of members from all three trust boards, typically senior figures. In some cases the chief executive post is filled by the same person across all the trust boards with the premise of having one key expert involved at all stages to ensure full visibility of performance.
This portions responsibility and duties more evenly across trusts, which is perhaps a fairer approach if trusts are smaller in national stature or of even standings compared to each other.
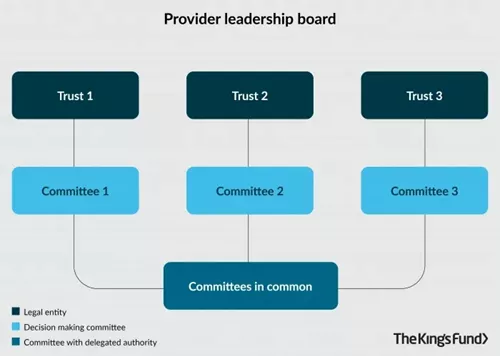
Provider Leadership Board:
Similarly to shared leadership, trusts in this instance report to committees (rather than a trust board) and then those decision-making committees report to a committee that includes the delegated authority.
Chief executives and directors will be part of this delegated committee, acting on behalf of their trusts when approved by their own committees.
The official NHS England guidance on working together at scale with provider collaboratives does lay out guiding principles for governance, as per the Health and Care Bill 2022. The paper states that provider collaboratives:
- must be underpinned by a shared vision and commitment to collaborate to deliver benefits of scale and mutual aid, doing what is best for people and populations across places
- should build on and enable existing successful governance arrangements; for some areas, arrangements may need to be strengthened rather than creating new arrangements from scratch
- should enable providers to efficiently reach decisions, which each organisation is committed to upholding, on topics that are within the collaborative’s remit
- should provide strong mechanisms for provider members to hold each other to account to ensure that decisions are reached and carried out and benefits of scale are realised at pace
- should ensure the needs and voices of local communities are a key consideration in all decisions and clinical leadership is embedded in programme delivery
- should make it clear how decisions are made, how disagreements are resolved, how funding flows to services within the collaborative’s remit, and how the collaborative is resourced
- should help streamline ways of working within and across systems; for instance, representatives of provider collaboratives are empowered to engage in conversations about services and transformations that are to be delivered at scale, rather than each individual provider needing to be consulted

Acute provider collaborative
Acute provider collaboratives are specific partnerships between those providers who handle acute care, which typically encompasses emergency care (A&E), urgent or critical care, pre-hospital care, and short-term stabilisation of an illness or injury.
North West London acute provider collaborative has their own detailed explanation about their remit. In their words, an acute provider collaborative can standardise protocols and processes, which allows staff to move more freely between partners to assist when required to support care delivery or to combat staff shortfalls and the workforce pressures that come with absences or job vacancies.
NWLAPC also extols the virtues of such collaboration and cooperation as being a great way to provide further skills training and development to staff, and to see which clinicians are best suited to handle more management and leadership duties – key responsibilities and authority for ensuring standards, care quality, and the development of new staff.
The King’s Funds’ article on provider collaboratives cites Royal Free London as one of the first acute care collaborations – alongside Barnet and Chase Farm. Similarly to North West London, this collaboration cited the reduced variation of clinical services, as well as a reduction in costs by reducing duplication of care and reducing spend on agency staff when the shared pool of clinicians has a better capability to cover shifts.
Mental health provider collaboratives
Mental health provider collaboratives are another specialist type of collaboration for NHS trusts. NHS England describes them as “a shift in the approach to commissioning specialised mental health, learning disability and autism services.”
In the same way the goal of acute provider collaboratives is to reduce care overlap and increase care capacity, so too is this mental health strategy; seeking to ensure that mental health support is available but with equal provision for those with learning disabilities and those who are neurodivergent with conditions such as autism spectrum disorder (ASD).
Many of the people in these instances need specialist or alternative healthcare, but with strict budgets and well documented difficulties recruiting into the NHS, the approach to utilise mental health provider collaboratives helps meet these needs, and often at a community level rather than in a hospital. The collaboratives cover both community forensic mental health care services and Child and adolescent mental health services (CAMHS).
The NHS Long Term Plan has a dedicated NHS mental health implementation plan for 2019 – 2024. This official document states: “The growing role of NHS-led provider collaboratives in delivering whole pathways of care for populations have already started to show us that short and purposeful stays, close to home linked with quality community services can deliver improved patient care.”
Provider collaborative guidance
The NHS Long Term Plan, and the more recent Health and Care Bill 2022, have given NHS trusts in England a great blueprint for how to establish provider collaboratives and to increase care provision and quality whilst reducing duplication of care and services, thus saving vital funds.
The next step is continued digitisation. The NHS is still slowly and surely overhauling outdated software or introducing new solutions never before available to help automate care processes, and organisations like The Access Group are the providers helping the NHS optimise their services and introduce greater efficiency and cost-effectiveness in day-to-day operations.
At Access we have several examples of this, with solutions such as Rio EPR, bed management, or technology-enabled care (home care devices and wearables). We have been working keenly with NHS trusts, but it is with a combination of intelligent software solutions from all manner of providers that these collaborations will achieve all they can.

