
What is the HSE in Ireland?
The HSE – Health Service Executive – is Ireland’s national health service. It is their equivalent of the UK’s NHS and a public provider of health and care services.
People who have been a resident in Ireland for a minimum of one year are entitled to public healthcare for free through the HSE, but usage is still permitted for those with less than one year in the country for a fee. Similarly, visitors with NHS cards, European health cards, or health insurance packages can also get discounted or free care too.
HSE history
The Health Service Executive (HSE) launched on January 1, 2005. It was ratified in the Health Act 2004, and replaced the previous setup which was health and care provision via 10 regional ‘Health Boards’ and the Eastern Regional Health Authority – as well as numerous other organisations or agencies.
Former health minister Dr James Reilly TD announced restructuring changes back in May 2013 for Irish public hospitals, in a drive to improve care outcomes. The groupings were as follows:
- Dublin North East
- Dublin Midlands
- Dublin East
- South/South West
- West/North West
- Mid West
More reorganisation was announced for 90 primary care networks in October 2014, and the above hospital regions were renamed in 2015.

Health Service Executive areas
The Health Service Executive is broken up into six parts to cover the Republic of Ireland, as seen on the official HSE graphic above:
- RCSI Hospitals (formerly Dublin North East)
- Dublin Midlands Hospital Group
- Ireland East Hospital Group (formerly Dublin East)
- South/Southwest Hospital Group
- Saolta University Health Care Group (formerly West/North West)
- UL Hospitals Group (formerly Mid West)
The Irish Times reported back in October 2014 about the new structure for local services. Their article highlighted the further structural changes, with nine Community Health Organisations being established across Ireland to replace the previous setup of 17 Integrated Service Areas.
These organisations are responsible for non-hospital services, and in the present day are made up each of 10 Primary Care Networks. The tactic is to roughly split the population of each PCN to handle approximately 50,000 citizens; providing them services for health, social care, mental health, and other aspects of wellbeing.
HSE management structure
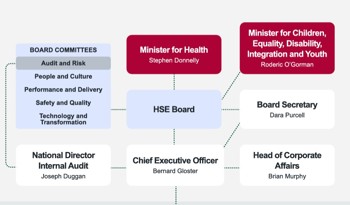
Ireland’s Health Service Executive is led by Director-General Bernard Gloster, who has been in position as head of the HSE since March 6th, 2023.
Gloster reports to the HSE board, who answer to Stephen Donnelly TD (Teachta Dála), the Minister for Health and the elected member of Ireland’s parliament (Dáil Éireann) for Wicklow. Donnelly then reports to the government’s cabinet and the Irish Taoiseach (Prime Minister) – currently Simon Harris.
As the image above shows (courtesy of the HSE), there are other directors and heads of branch, as well as board committees and the Minister for Children and Equality, Roderic O’Gorman, who also hold the HSE to account.
Below Gloster is then the Executive Management Team, comprised of roles including but not limited to Chief Strategy Officer, Chief Information Officer, Chief Clinical Officer, Chief Financial Officer, and National Director of Human Resources.
The CEOs of the six previously mentioned hospital groups report to National Director of Acute Operations, Mary Day. The Chief Officers of the Community Healthcare Organisations (nine areas) report to National Director of Community Operations, Schemes & Reimbursement - David Walsh.
You can view the full executive management structure of the HSE on their website.
The core structure of the HSE is compartmentalised into three ‘service delivery units’. These are:
- Primary, Continuing and Community Care: GP surgeries and social services, for example.
- National Hospitals Office: Hospitals and ambulances.
- Population Health: Overall wellbeing management and population protection via health promotion and support campaigns.
These three areas handle the day to day health and care provision for Ireland, as well as longer term objectives, and employ over 100,000 people in order to achieve the HSE’s goals and duties.
HSE services
The duties of HSE Ireland correspond directly with the services provided. We have already shown how there are three service delivery units. These seek to promote good health, prevent illness, and provide diagnosis and treatment where possible – all done through hospitals, GP surgeries, and community care.
HSE Fair Deal Scheme
One service the HSE in Ireland provides is the Fair Deal Scheme. This is for residential care in a nursing home. Similar schemes through local councils and authorities exist in the UK nations individually also, but the scheme is simple: the HSE will assess the eligibility of a person needing residential care. If approved, the HSE will then pay a proportion of the care bill. Their own website gives the example of a €1200 a month care bill. Based on means testing, the HSE determines the client (or their family) can and thus should pay €400 in contributions. The HSE will then settle the remaining €800 balance.
HSE finance
HSE Ireland is a big organisation. Its expenditure, based on Ireland’s GDP, was approximately 6.1% as of 2022. The Irish government gives €16.05 billion funding per year to the HSE, which the executives such as Bernard Gloster are then tasked with spending appropriately in order to provide the largest breadth of care whilst maintaining the highest standards.
Transparency is readily available in the HSE however. The RCSI Hospital Group details their share of this funding to be €1.272 billion according to their About Us page. They also detail staff employed and their assigned population figure – 875,000 people across five counties.
Prior to Covid-19, the HSE had a €60 million surplus. This expanded to €200 million in 2020 due to government funding for the pandemic, but has since flipped to a deficit in both 2021 and 2022 - €195 million and €185 million respectively.
Financial stability and the affordability of services is a big challenge for the Irish government…

HSE challenges
The cost of the HSE is a challenge that faces the Irish government. The media and political parties have repeatedly criticised the Health Service Executive of being “top-heavy” and “inefficient” due to bureaucracy and poor management.
There have also been dramatic issues such as the CervicalCheck cancer scandal back in 2018 – an incident relating to incorrect cancer diagnoses in 2008 that resulted in large settlements with patients.
Ireland HSE cyber attack
On a similar scale was the 2021 cyber attack on Ireland’s HSE systems. A ransomware attack infiltrated the Health Service Executive computer network and demanded payment to unlock the system. To this day it is the largest known digital attack on a health service and the largest against the Irish state, though there was no confirmation of who the perpetrators were beyond suspicions of the Russian Federation.
Recommendations have been made by the Irish parliament however, with public documents available about the examination of the 2020, 2021 and 2022 financial statements for the HSE. The Committee of Public Accounts delivered six recommendations to the HSE:
- Implementation of the HSE’s Integrated Financial Management System
- Child and Adolescent Mental Health Services (below standard currently)
- Oversight and governance of Section 38 and Section 39 agencies
- Procurement of ventilators during the COVID-19 pandemic, and obsolescence of COVID-19 vaccines
- Recruitment across the HSE, and high remuneration of staff at the organisation
- Collapse in the availability of public dental services
HSE statistics
Statistics and figures are the ultimate judgement of the HSE’s performance.
Professor Martin Curley, writing in the Irish Times in 2023, provided his opinion on why Ireland’s health system is one of the lowest performing in the northern hemisphere. Professor Curley described it as “the canary in the coal mine”; the HSE has excellent clinicians and provides good care, but in his words the HSE is ranked as 80th in the world as a health service provider.
Except he’s wrong. The CEOWORLD magazine Health Care Index for 2023 has Ireland in 20th place, just behind France. For 2024, Ireland has jumped up markedly to sixth place; ahead of Germany in 8th, Japan in 13th, France in 25th, and the UK in 27th.
Not all of Professor Curley’s opinion piece is incorrect. He states that:
- It remains the only western European country without universal coverage for primary care. This is correct, but has been explained regards Ireland’s complex approach to affordable care and provision.
- Since the introduction of Slaintecare, Ireland’s wait-lists have almost doubled despite record and increasing spending. This was confirmed by the Irish Independent in June 2023, though it did not suggest double – it says approximately 500,000 people are waiting; a figure the government contests is due to the Covid backlog of appointments.
- A highly touted €350 million waiting-list reduction plan last year resulted in a paltry one per cent reduction. We have been unable to verify this claim.
- In newly-released figures Eurostat ranks Ireland currently as the fourth worst in Europe for excess mortality at 12.2 per cent, compared to a European average of 2.7 per cent. The source is legitimate, but does state it’s for April 2023 only.
There are better figures about the Health Service Executive though. According to the European Commission, HSE Ireland has overseen a sharp increase in life expectancy since 2000. The HSE annual report for 2022 confirmed this, with men typically living to 80.8 years old and women to 84.4 years old. The HSE has also managed to close the gap to 3.6 years from the 5.2 year gap in 2000.
Health Manager website also goes on to cite the following:
- Ireland has the highest self-perceived positive health status in the EU, with 82.1% of people rating their health as good or very good.
- Since 2012, the mortality rate from all causes of death has decreased by almost 16%. There has been a 15% reduction in the mortality rate from cancer, a 38% reduction in the mortality rate from ischaemic heart disease, and a 48% reduction in the mortality rate from stroke.
- There has been a reduction of 32% in the mortality rate from respiratory system diseases (excluding cancer of the trachea, bronchus and lung) since 2012.
Ireland still suffers with issues regards universal care, higher than average rates of respiratory disease, and waiting times, but these aren’t unique problems to the Republic. The conclusion we can make from all this is that no health service is perfect, and critique should always be welcomed, but the stats don’t lie – Ireland’s HSE is doing a good job for the public.
