
Discharge Process from Hospital – What is it?
A hospital discharge is the process of allowing a patient who has been admitted to the hospital to return home safely. To be discharged safely from the hospital, every patient will undergo a discharge assessment to determine whether a patient has a minimal or complex discharge.
- Minimal Discharge – Where a patient needs little to no care after leaving the hospital
- Complex Discharge – Where a patient needs more specialised care after leaving the hospital
Every hospital will have its discharge policy, but every hospital will follow the new Discharge to Assess procedure to enable social care workers to assess patients at home or in the community rather than in a hospital setting.
Alternatively, patients can also discharge themselves, known as discharged against medical advice (AMA).
Whether it’s a minimal or complex discharge process all patients have to undergo an assessment to ensure all patients return home safely to increase independence and prevent readmissions.
Learn more about the Discharge to Assess today.
What causes delayed discharge from hospitals?
Often when a patient is discharged from the hospital the best place for them ideally is to continue receiving the care and support needed in the comfort of their own home. However, most discharge procedures tend to be a bit more complex.
The list below some of the main reasons for delays in discharge processes in hospitals:
Here's your section transformed into a listicle format:
1. Bed Blocking:
- Often attributed to patients, bed blocking actually stems from limited care and support available in patients' local areas.
- This scarcity of care creates delays in discharge as there's nowhere deemed safe for patients to go, increasing pressure on hospital and care home beds.
2. Health and Social Care recruitment and retention challenges:
- The private sector, a major provider of adult social care, faces a staffing crisis due to recruitment and retention challenges.
- The challenges across health and social care recruitment and retention lead to higher demand, longer hours, pandemic-related strain contributing to staff burnout.
- The Local Government Association (LGA) 71% of councils struggle to recruit adult social care workers, and they have called on the government to deliver a long-term care workforce strategy to tackle the issues of staff recruitment, retention, and pay
- Skills for Care reported vacancy rates in local authority adult social services reached 10.2% in May 2022, disrupting public health services.
- The LGA’s 2022 Public Health Annual Report published with the Association of Directors of Public Health (ADPH) stated that more than half say their public health services are being disrupted due to staff shortages.
3. Funding Pressures:
- Limited budgets strain councils, hindering long-term staffing and development plans.
- Without adequate funding, delivering high-quality care becomes increasingly difficult as councils struggle to confidently make plans to develop or recruit the workforce needed to deliver the best quality care
4. Outdated Processes in Care Placement:
- Long, manual processes for commissioning, regulation, and onboarding care providers weaken and delay the efficiency of finding suitable placements.
- This can lead to inefficient settings or prolonged wait times for suitable placements, sometimes resulting in patients being placed in incompliant care settings that don’t meet their needs, or meet the local authorities’ responsibilities under the Care Act.

What are the impacts of delayed hospital discharges?
Ultimately delayed hospital discharge impacts three different groups in a variety of ways:
- Patients and their loved ones
- Hospitals
- Local Authorities
1. Patients and their loved ones
- Patients are left in hospital longer than they need to be
- An increased risk of stress and uncertainty for patients and their loved ones about the next steps of their patient journey
- Decreased morale and mood
- Decreased patient outcomes
- Increased risk of readmissions
2. Hospitals
- Risk of running out of hospital beds and overflow beds
- Bad for patient flow
- Increased pressure on staff to meet targets
- Increases hospital and health system costs
- Reputational damage
- Difficulty finding space for new arrivals
- Increased demand increases risk of working longer hours, burnout, and healthcare professionals leaving the profession altogether which in turn worsens the cycle further
3. Local Authorities
- Increased pressure to find appropriate care and continuing healthcare placements efficiently and quickly
- Stretches budget and capacity
- Increased risk of not having enough resources to meet the demand
- Risk of losing data or information from long outdated processes leading to reputational damage and hefty fines
- Risk of providing poor quality care which does not meet the regulatory requirements under the Care Act
- Increased demand increases risk of working longer hours, burnout, and social care professionals leaving the profession altogether which in turn worsens the cycle further
What is the cost of delayed discharge from hospitals?
It has been argued in previous years that delayed discharge procedures cost the NHS £900 million. This was a figure declared before the pandemic and the argument then was that the figure could be higher.
Now with ambulance handover times being at the highest it’s been in 2023, and over 14,000 patients medically fit in hospitals not being discharged, it wouldn’t be surprising if that figure is higher as the delays continue.
The cost of looking for alternative settings, and paying extra staff to meet the demand, including locum and relief staff all adds extra financial strain onto the NHS.
The delayed discharge process also adds financial pressure to local authorities. This, in turn, stretches their limiting budgets further exacerbating the challenges they have already.

Improving discharge delays in hospitals - What are the government doing?
In order to tackle the delays in hospital discharges, the UK government announced that £250 million of funding would be given to speed up hospital discharges.
The funding was to buy short-term placements in community settings, including care homes, to fund stays of up to 4 weeks of extra care per patient, with an end date of January 2024.
£200 million of the funding was given to local authorities to ‘bolster’ social care workforces to increase their capacity so they take on more patients.
An additional £50 million of capital funding was given short-term to upgrade and expand hospital discharge lounges, ambulance hubs, and facilities for patients about to be discharged to tackle queues of paramedics waiting to handover patients.
Local authorities were told they could spend this money on initiatives that would have the greatest impact in their area on reducing discharge delays.
In order for this to be successful, the government encouraged local authorities and integrated care boards (ICBS) to work together to agree on their spending across their regions so more tailored solutions that benefit both parties can be introduced to speed up discharge processes in their local area.
The King’s Fund published a consultation report on hospital discharge funds in November 2023 which spoke with key stakeholders about their experience. With a general election expected in 2024 though, it is unclear if the incumbent government will renew the scheme for 2024/25.
Now, in 2024, guidance and outlines have been amended to reflect section 82 of the NHS Act 2006 to ensure that NHS bodies and local authorities must cooperate the discharge models that best meet local needs to ensure they are both effective and affordable with the budgets available.
Here this updated guidance as well the 4 pathways under the discharge to assess model helps to formalise methods to improve discharge processes.
Improving hospital discharge process - What was the reaction to the government's proposal?
Warnings about adult social care requiring more funding have been stated for a long period. also warned in July 2022 how this would be necessary so it could have a significant impact to reduce winter pressures.
There have been many concerns that this immediate committed funding is being too heavily reliant on care homes and that the funding should go towards making home care packages in a hospital discharge the priority. ADASS has argued that defaulting to discharging patients to care homes runs the risks of individuals being inappropriately placed and that patients will end up staying in residential homes indefinitely.
ADASS were not the only one to voice this concern, David Fothergill the community wellbeing board chairman for the LGA, has also said that this crisis has been caused due to under-funding from across the last decade and that more long-term methods in easing pressure needs to be seen as an essential task.
There are also concerns that with about 500,000 people awaiting social care needs assessment or care packages, focusing this extra funding on discharge processes could neglect people’s needs in the community and increase the risk of being self-defeating.
The Department of Health and Social Care however believed it will support thousands of medically fit patients to be discharged. If successful, it was also deemed to reduce pressure on A & Es and speed up ambulance handovers by allowing patients to be admitted to wards from emergency departments quickly.
The Health Foundation argues that often when extra short-term funding like this comes into play there often isn’t enough time for local authorities to utilise the funding strategically so often local authorities do not see the benefits they could see.
A UK Government survey in 2021 on workforce capacity fund for adult social care found that 55 out of 59 local authorities surveyed found the timeframe to use the workforce capacity funding in 2021 insufficient.
These mixed reactions show that despite different providers and stakeholders having different opinions on the discharge fund, what local authorities need is more time. This isn’t something the fund offers though, and local authorities need to seek alternative ways to be better prepared for future demand; to develop a more strategic approach to reduce hospital discharge delays.
Following the uncertainties of future funding, in January 2024 it was announced an additional £500 million in social care funding. The aim of this funding is to encourage local authorities to use this funding to drive innovation and increase performance. Through digitally transforming their social care services more medically fit patients can be discharged from hospital sooner back to their own homes with the appropriate social care they need to continue to recover. This, in turn, allows local authorities to deliver stronger proactive care that is catered to every individual and adapt as needs change by storing all information in one centralised place.
Now in 2024, with the average days from being discharge ready date to the date of discharge reducing by 0.4 days in the last four months from 6.4 days to 6 days, it is clear that what local authorities need more of is time. However, this is something that the fund did not offer and therefore local authorities needed to and still do need to seek alternative ways to be better prepared for future demand, to develop a more strategic approach to reduce hospital discharge delays.
Discover our local authority software today to see how we can help digitally transform your services to improve quality, drive innovation, and most importantly reduce discharge delays and dependency on residential care homes.

How to improve the discharge process in hospitals
For local authorities to be in the best place to reduce hospital discharge delays, the first thing they must address is what are the main issues causing the delays in their community. It is crucial for local authorities to set targets and be strategic in their approach and work collaboratively with nearby local authorities to ensure no patient goes without the care they need, but until those issues are highlighted the next steps are more than likely to be unsuccessful.
Local authorities must set targets, and be strategic in their approach by working collaboratively with nearby local authorities to ensure no patient goes without the care they need.
Improving the discharge process in hospital will have a domino effect on the problems associated with the delays. One of the best ways to reduce hospital discharge delays is in investing in different technological solutions and digital tools which best suit your council’s needs.
There is a wide range of technology which can help local authorities achieve their goals in reducing discharge delays including:
- Maintaining patient’s independence
- Mitigating risks and improving the quality of care
- Improving future forecasting
- Having a better strategic approach
- Improving the patient experience

1. Maintaining patient's independence
The power of technology enabled care
There are many different strategies councils and local authorities can follow, but the biggest concern is to follow a home-first principle. This will ensure that where possible when a patient is discharged they can remain independent and healthy in their own home.
Investing in technology-enabled care is just one example of supporting this. Technology enabled-care and digital telecare solutions provide an eco-system of solutions which offers both sustainable and preventative care.
At The Access TEC we offer more than just a digital alarm system. We combine traditional reactive alarm functionality with proactive digital monitoring so daily activities of life can be monitored and alerts can be sent out to both reassure and alert loved ones and care providers when needed.
Both local authorities and end-users can benefit from using digital telecare as our unobtrusive monitoring ensures that regardless of where a patient is discharged to they can remain independent for as long as possible, as long as it is deemed safe to do so.
One of our customers, Airtel Vodafone, worked with the Government of Jersey to encourage a mass roll-out of technology-enabled care across Jersey and found that through using our digital telecare and working collaboratively, over 95% of self-funding users chose to switch to the new service.
We understand that interoperability is highly important in the health and social care sector to help local authorities deliver better joined-up person-centred care. Our digital telecare helps address this gap in the health and social care market to help individuals stay independent for longer, reassure their loved ones in what has been a stressful time, whilst helping reduce discharge delays.
Our latest integration with our care planning software helps ease the transition to returning home to not only reduce discharge delays but prevent readmissions. Care workers can have full visibility of the smart alerts and alarms set up in the Access Assure Hub in our care planning mobile app to have all the information needed in one place.
Here better proactive care is enabled as staff feel empowered to make better data-led decisions that put the individual at the centre of everything they do. Patients also feel more comfortable continuing with their recovery in the comforts of their own home with the reassurance that help will be there before something more critical happens to make recovery easier and avoid readmission.
The power of virtual wards
Another way independence can be maintained to help reduce discharge delays and hospital readmissions is through utilising virtual wards.
Virtual wards are a way of monitoring care provided away from a hospital ward, meaning that when a patient is discharged they are still receiving regular checks to monitor their recovery at home. This, in turn, enables individuals to recover in a more comfortable and relaxed environment reducing stress and improving their recovery time.
Here healthcare professionals can be a lot more flexible in how they support individuals and complete their visits whether in-person or virtually via video calls. Individuals that can do themselves can also record their vital signs to report back.
Not only do virtual wards help to speed up the discharge process therefore, they in turn are cost-effective, reduce congestion and reliance of hospitals and care homes, remove the risk of bed-blocking, and help health and social care professionals better manage workloads to prevent burnout, whilst enabling individuals to become more independent.

2. Mitigate risks / improve care quality
One reason why patients are delayed in their hospital discharge is because the available care placements may not be safe for them.
Investing in technology that thoroughly checks, assesses, and flags risks with care providers is a way to reduce delays whilst still maintaining the rigorous assessments expected.
Using digital dashboards is a great way to track your provider markets and make note of which providers will suit the right patient after their discharge assessment. Having all this information on your provider markets in one place makes it easier to spot trends and potential risks so that they can be monitored across care type and location.
We go a step further at The Access Group and our Risk Profiler solution brings together all this information and offers a variety of sophisticated filtering options so risks can be monitored according to the patient’s needs as well as your local areas needs too. Here regulator checks can be managed to ensure no individual receiving care whether it is in a residential home or with domiciliary care is put at risk.
Our Social Care Landscape module also helps you assess key challenges across nearby local authorities as well as your own so you have everything you need to know about demand, spend activity, capacity, and risk altogether so contingency plans can be put in place so everyone receives the care they need.
Worcestershire County Council found through assessing spend activity across different client groups and services across the market, they have been able to gain valuable up-to-date insight in how placements costs compare locally, regionally, and nationally.
This in turn, helps to determine the best care placement possible in real-time efficiently to reduce discharge delays and ensure all individuals receive the best quality care to make improving patient outcomes a top priority.
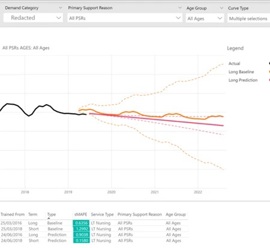
3. Improve future forecasting
Being able to accurately estimate future demand is imperative for local authorities to commission the right capacity of care needed across the adult social care market including discharge care plans.
One way to do this is through investing in demand modelling technology, so both demand and capacity can be consistently delivered now and in the future without putting anyone at risk.
The benefits from using demand modelling technology include being able to make highly accurate predictions about future demand. This then reduces the element of surprise if a patient needs a particular care plan, as through demand modelling your local council will already have an accurate estimate of how many other individuals need a similar care plan.
We conduct this through combining statistical forecasting techniques with artificial intelligence to manage unexpected events more efficiently and predict areas of risks to ensure the right provisions are in place without going over budget.
Middlesbrough Council, for example, have found using demand modelling has improved how their data is analysed to their improve future planning. Now they have up to 99% accuracy in their future forecasts to ensure they have the capacity to facilitate any discharge care plan that may arise.
Demand modelling helps reduce the discharge delay therefore, by helping local councils be prepared and commission the right levels of resources needed so they are no surprises or delays when a discharge care plan comes through.
4. Having a better strategic approach
For local authorities to get the most out of their awarded funding they need to be proactive and have strategic commissioning.
One of the most important things local authorities can do to is digitally transform their procurement processes. Moving from long, outdated manual or paper-based processes is one of the best ways to save time searching for appropriate care placements for patients.
Through digitising your procurement process for continuing healthcare, the number of manual tasks can be reduced and the whole process can be streamlined via a single system.
Digitising your procurement process gives you full visibility of the provider market, so patients can be placed with fully compliant providers that meet their specific needs and are available when you need them.
At Access Adam Care Commissioning, we list the providers in real-time according to your needs. This way the highest ranking provider will feature at the top of your rankings automatically.
Midlands Lancashire Commissioning Support Unit (MLCSU) has found through digitising their procurement process they have better access and control of their provider market to create more effective patient pathways to improve outcomes, at a better value for money.
One resident found they were able to place their family member into their preferred care home which matched their needs better than what they were first offered, saving themselves over £5000 per annum in the process.
Digitising your procurement processes therefore helps reduce discharge delays as our commissioning platform helps find you the best provider by saving time and automatically selecting providers that best meet your care needs.
5. Improving the patient experience
By achieving all of the above a local authority is naturally improving the patient experience, but it’s also important to include patients in the decision-making process.
This is known as patient engagement, and is a great way to better educate patients so that they have the confidence to manage their own health in a more effective way. Including people in their own health and care journey – especially when it comes to decision making – benefits a patient’s mental health and their willingness to engage with clinical support.
This leads back to better care quality too, as a willing patient is onboard with their own treatment plan or care proposals and engaging with the support provided.
Hospital admission and discharge process – How can technology help?
In this article, we have reviewed what a typical discharge process can look like by explaining the differences between minimal, complex, and AMA discharges, as well as the main causes of hospital discharge delays including the impacts that has on patients, their families, hospitals, and local authorities.
We have discussed how investing in different technological tools can help local authorities best prepare for patients' care plans once discharged so they have the capacity and the resources to deliver the care they need.
By explaining what solutions we offer at The Access Group we have demonstrated that we have a wide variety to choose from according to your goals and care needs.
By encouraging collaborative working and co-production with other local authorities and organisations, we can ensure that resources are shared to enable individuals who have already been waiting to be assessed don’t get delayed further by the increase in demand to establish better resource allocation across the market.
For more information on how technology can help reduce hospital discharge delays and improve patient outcomes discover our local government software today.
Contact us and see how we can help you reach your goals so you can deliver the best continuity of care possible to the residents in your local community to reduce discharge delays and prevent avoidable hospital admissions and readmissions.

