
Empowering Individuals with Greater Control Over Care
The ARF prioritises providing individuals with greater autonomy in managing their care through digital tools. These innovations ensure care recipients can better communicate their preferences and self-direct their support, creating a more person-centered care system.
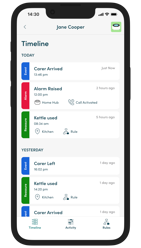
• Digital tools, such as apps, can support people to have more choice over their care, particularly for those receiving direct payments or using an Individual Service Fund.
• Direct payments and personal budgets are a vital way in which people can have more choice and control over their care and support.
• Innovative tools can support people to have better access to up-to-date, relevant information and advice and help people feel supported to make informed decisions about the support that suits them. Research by IMPACT found that in addition to accessible information, visual tools can also help people understand how their support package is designed and how their personal budget is being spent.
Key Initiatives:
• Self-Assessment Platforms: Digital tools are enabling users to evaluate their care needs and access tailored resources. Councils like Medway and Kent are leading in this area by developing intuitive platforms that simplify the care management process.
• Real-Time Communication Tools: Video consultations and remote monitoring technologies , as seen in Worcestershire, help users stay connected with care providers while minimizing unnecessary travel and stress.
• Tailored Service Delivery: Apps and systems give individuals the power to schedule appointments, adjust care plans, and communicate preferences directly with care teams.
By empowering individuals to take charge of their care, these tools align with broader national goals for a National Care Service that values autonomy and efficiency.
Building Resilient Local Communities
The ARF emphasises investing in local area networks to support prevention and promote wellbeing, enabling individuals to age well in their communities. A community-first approach reduces dependency on institutional care while fostering a sense of belonging and support.
The Darzi report highlights that while other sectors have gone radical digital transformations over the past decade, the NHS is still in the early stages of full embracing digital solutions within health and social care. This presents a significant opportunity for improvement, with the potential to enhance for its poor performance, efficiency, and patient outcomes across the system. .
Since at least 2006, and arguably for much longer, successive governments have promised to shift care away from hospitals and into the community,’ said Lord Darzi. The Royal College of Nursing (RCN) predict that nursing numbers will more than half by 2029 and has called upon Labour to prioritise investments in district nursing professions as these people play an integral role in keeping people well within the community and preventing hospital admissions.
One way of supporting people in local areas is to develop age-friendly community initiatives. Age-friendly communities are places where age is not a barrier to living well and where the environment, activities and services enable older people to:
• have opportunities to enjoy life and feel well
• participate in society and be valued for their contribution
• feel safe, comfortable and secure at home
• access high quality health and social care
Key Focus Areas:
1. Preventative Health Programmes
Local councils are adopting community workshops focused on fitness, mental health, and social connection, ensuring older adults remain active and engaged.
Initiatives like those in Lincolnshire provide respite opportunities for unpaid carers through arts, heritage, and outdoor activities.
2. Age-Friendly Community Design
Accessibility improvements in public spaces, including better mobility support and integration of care services into community hubs, allow individuals to live independently for longer.
3. Community Network Strengthening
Collaboration between local authorities and community organisations ensures seamless access to services such as transportation, meal delivery, and companionship programmes.
These efforts help individuals thrive within their communities, reducing hospital admissions and improving overall quality of life.
Involving Unpaid Carers in the Discharge Process
Unpaid carers play a vital role in the adult social care system, particularly during transitions such as hospital discharges. The ARF focuses on outreach and support for carers to ensure they are involved in care planning and adequately equipped to meet post-discharge needs.
The total number of patients in acute hospitals who were ready to leave hospital but were delayed has increased by 43% from an average of 8,545 patients per day in June 2021 to 12,223 patients per day in June 2024. At its peak, in January 2024, there were 14,096 patients delayed in hospital.
Innovations in Carer Support:
• Hospital Discharge Coordination
Improved planning processes ensure carers are active participants in discharge meetings, giving them a clear understanding of their loved ones’ care needs.
Digital platforms provide carers with up-to-date discharge plans and ongoing communication with healthcare professionals.
• Training Programmes
Educational resources equip carers with the skills and knowledge required to manage specific medical conditions or rehabilitation processes at home.
• Respite Opportunities
Dedicated respite care programmes allow carers to recharge while ensuring continuity of care for patients. These programmes are particularly valuable post-discharge, a period often marked by high stress for carers.
By integrating carers into every step of the discharge process, the ARF enhances care continuity and reduces readmission rates.
Expanding Social Prescribing
Social prescribing connects individuals with information, advice, and community resources to address social determinants of health. This holistic approach promotes wellbeing and prevents crises by empowering individuals to access support beyond traditional healthcare.
Implementation Highlights:
• Link Workers in Local Communities
Dedicated professionals help individuals navigate services such as mental health counselling, exercise groups, and peer support networks.These workers act as a bridge between healthcare and community-based resources.
• Digital Social Prescribing Platforms
Apps and online tools enable individuals to explore available programmes and self-refer to activities that align with their interests and needs.
• Enhanced Community Resources
Investments in local organisations, such as gardening clubs and creative arts groups, provide meaningful engagement opportunities for those at risk of social isolation.
Social prescribing empowers individuals to take proactive steps toward better health while fostering resilience within communities.
Conclusion: A Holistic Approach to Adult Social Care
The Accelerating Reform Fund 2024–2025 exemplifies a bold and innovative approach to tackling the challenges in adult social care. By focusing on:
1. Empowering individuals with digital tools,
2. Building resilient communities,
3. Supporting unpaid carers during critical transitions, and
4. Expanding social prescribing;
The ARF sets a strong foundation for a sustainable and equitable care system. These targeted investments ensure that care is not only accessible but also person-centred , responsive, and integrated into the fabric of local communities.
For more details on ARF-supported initiatives, visit GOV.UK or Community Care. These priorities reflect a commitment to driving impactful, long-term reform in England's adult social care landscape.
